
![]()
Types of Assessment Methods
Objective Structured Clinical Examination
- What are Objective Structured Clinical Examinations?
- Structure of Objective Structured Clinical Examinations
- Advantages of Objective Structured Clinical Examinations
- Disadvantages of Objective Structured Clinical Examinations
- How to design a good Objective Structured Clinical Examination?
- Marking Rubrics
- Web References and Resources
What are Objective Structured Clinical Examinations?
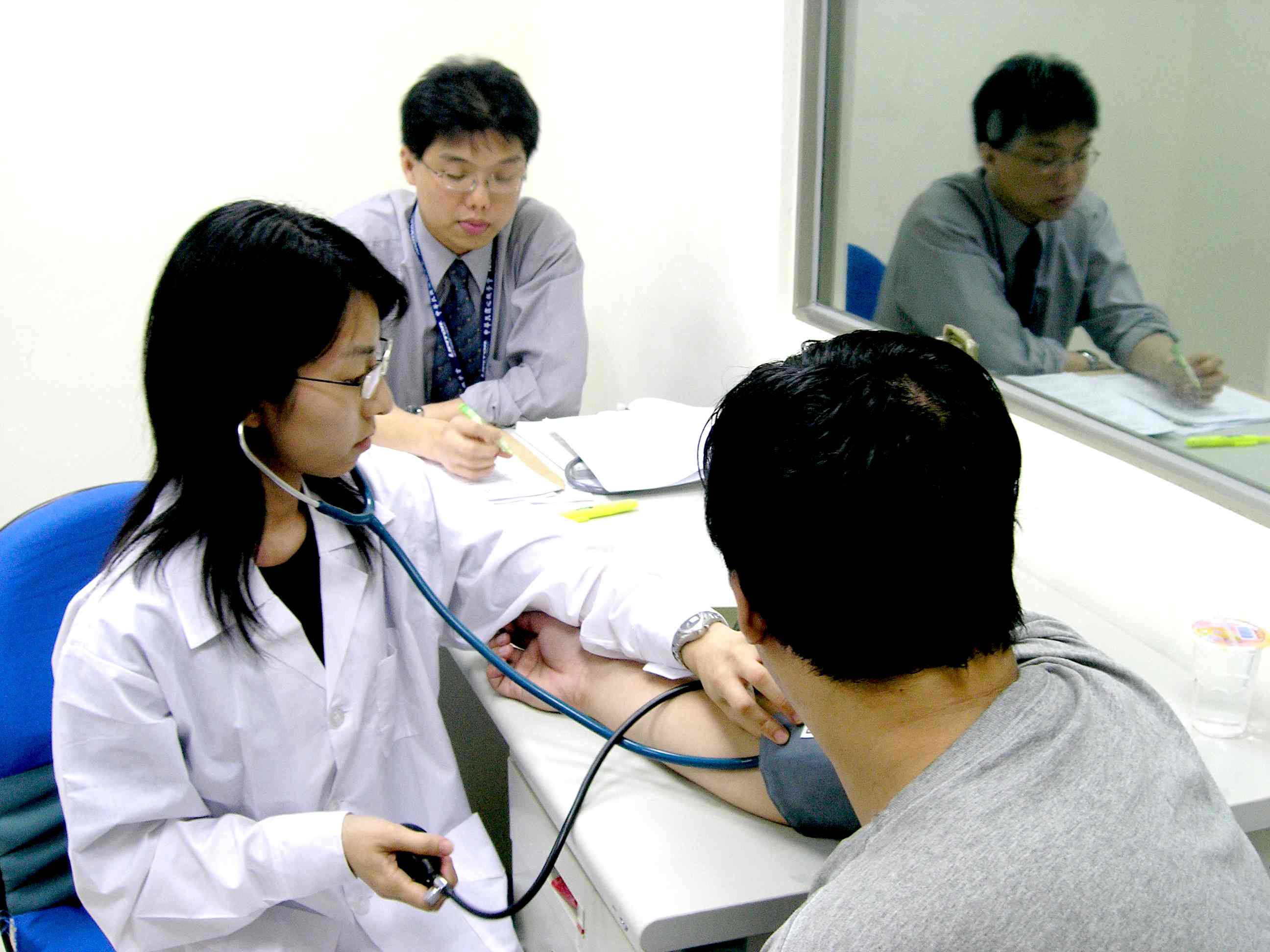
Objective Structured Clinical Examination (OSCE) was introduced by Harden and his colleagues in 1975. In an objective structured clinical assessment, a series of stations in an examination room is set up to examine students. At each station, students may be asked to carry out a procedure, which may involve taking history, performing preset clinical tasks and diagnosing patients' problems. When performing the clinical tasks, students may often interact with 'patients', who may be healthy volunteers or mock patients. Students also have to answer questions based on their findings and their interpretation. Students are observed and scored at some stations by examiners with checklists.




Structure of Objective Structured Clinical Examinations
Objective Structured Clinical Examination consists of a series of stations that examines the competency of students in taking histories, practicing specific clinical tasks, and interpreting some clinical data. There are two types of stations in this assessment method:
- Practically-based - Students are given a written instruction and have to carry out a procedure.
- Question-based - Students have to answer questions on their findings at the previous station and interpret these findings. The questions may be open-ended or of multiple-choice type.
Students are assessed by examiners through a previously-determined, objective marking scheme. OSCE can be adapted into other disciplines such as science and engineering.
| Declarative |  |
|
| Y | Functioning | |
| Y | Take Time to Set | |
| Y | Take Time to Answer | |
| Y | Take Time to Correct | |
| Y | Take Time to provide Feedback | |
| Suitable for Large Class | ||
| Can substitute with Computers | ||
| Passive | ||
| Y | Active | |
| Y | Process Oriented Method | |
| Y | Product Oriented Method | |
| P = Possibly Y =Yes | ||
Advantages of Objective Structured Clinical Examinations
- Provides a uniform marking scheme for examiners and consistent examination scenarios for students.
- It provides an authentic way to assess medical students including pressure from patients.
- Generates formative feedback for both the learners and the teaching program. Immediate feedback collected may improve students' competency at subsequent stations and even enhance the quality of the learning experience.
- Minimizes the effect of cueing: When students go to a station, they will need to diagnose patients' problems or carry out some clinical procedures. When they go to a subsequent station, they have to answer some questions relevant to their diagnosis or clinical tasks. However, students cannot go back to correct any mistakes or omissions on what they did in the previous station.
- More students can be examined at any one time. When a student is carrying out a procedure, another student who has already completed that stage is answering the question at another station.
- In the Objective Structured Clinical Examination, the setting is more controlled (only two variables exist: the patient and the examiner) and a more objective assessment of the student's clinical competency can be made.
- Provides more insights about students' clinical and interactive competencies.
- It can objectively assess other important aspects of clinical expertise, such as physical examination skills, interpersonal skills, technical skills, problem-solving abilities, decision-making abilities, and patient treatment skills
- It requires an extensive amount of organising.
- It is expensive in terms of manpower, resources and time (such as number of examiners, patients, and even space of examination room)
- It may discourage students from looking at the patient as a whole because the students' knowledge and skills are being put into compartments.
- The assessment examines a narrow range of knowledge and skills and does not test for history-taking competency properly. Students only examine a number of different patients in isolation at each station instead of comprehensively examining a single patient.
Steps in developing an Objective Structured Clinical Examination:
- Decide the types of skills to be examined
- Decide the types of assessment (such as a uniform checklist)
- Consider the number of skill assessment stations needed (it is recommended to have 10 to 15 stations, and six minutes for each station) because the length of the examination is determined by the number of assessment stations and the time each candidate will spend at each station.
- Allocate resources for the examination (such as space for examination rooms, marking sheets and plastic models)
- Prepare the staff resources needed (including examiners, timekeepers and patient/volunteers)
- Determine/arrange the day/period of exam
- Conduct a review/evaluation of the arrangement of the exam after it is over
- To design concise marking schemes that focus on actions that distinguish between good and poor performance
- To provide marking scheme instructions on what students would do at each station for the examiners
- To provide instructions which outline exactly the task required at each station for students
Below is a sample of the OSCE rubric:
| MARKING RUBRICS | Excellent | Proficient | Average | Poor |
| Diagnosis: | Able to give an excellent analysis and understanding on the patients' problems and situations and applied medical knowledge to the clinical practice and determined the appropriate treatment | Able to demonstrate medical knowledge with a satisfactory analysis on the patients' problems, and determined the appropriate treatment | Showed a basic analysis and knowledge on the patients' problems, still provided the appropriate treatment | Only able to show minimal level of analysis and knowledge on the patients' problems, unable to provide the appropriate treatment |
| Problem-solving skills: | Able to manage the time to suggest and bring out appropriate solutions to problems; more than one solutions were provided; logical approach to seek for solutions was observed | Able to manage the time to bring out only one solution; logical flow was still observed but there was a lack of relevance of the flow | Still able to bring out one solution on time; logical flow was hardly observed | Failed to bring out any solution in specific time; logical flow was not observed |
| Communication and interaction with patients: | Able to get detail information needed for diagnosis; gave very clear and detail explanation and answers to patients; paid attention to patients' responses and words | Able to get detail information needed for diagnosis; gave clear explanation and answers to patients; attempted but only paid some attention to patients' responses and words | Only able to get basic information needed for diagnosis; attempted to give a clear explanation to patients but omitted some points; did not pay attention to patients' responses and words | Failed to get information for diagnosis; gave ambiguous explanation to patients |
| Clinical skills: | Perfectly performed the appropriate clinical procedures for every clinical tasks with no omission; no unnecessary procedure was done | Performed the required clinical procedures satisfactorily; committed a few minor mistakes or unnecessary procedure which did not affect the overall completion of the procedure | Performed the clinical procedures at an acceptable standard; committed some mistakes and some unnecessary procedures were done | Failed to carry out the necessary clinical procedures; committed lots of mistakes and misconception about operating clinical apparatus |
Web Reference and Resources
- Barman, A. (2005). Critiques on the objectives structured clinical examination. Annals Academy of Medicine Singapore, 34, 478-482.
- Carraccio, C., & Englander, R. (2000). The objective structured clinical examination: A step in the direction of competency-based evaluation. Archives of Pediatrics & Adolescent Medicine, 154, 736-741.
- Harden, R. M., Stevenson, M., Downie, W. W., & Wilson, G. M. (1975). Assessment of clinical competence using objective structured examination. British Medical Journal, 1, 447-451.
- Prislin, M. D., Fitzpatrick, C. F., Lie, D., Giglio, M. Radecki, S., & Lewis, E. (1998). Use of an objective structured clinical examination in evaluating student performance. Family Medicine, 30, 338-344.
- Selby, C., Osman, L., Davis, M., & Lee, M. (1995). How to do it: Set up and run an objective structured clinical exam. British Medical Journal, 310, 1187-1190.
- Sloan, D. A., Donnelly, M. B., Schwartz, R. W., & Strodel, W. E. (1995). The objective structured clinical examination: The new gold standard for evaluating postgraduate clinical performance. Annals of Surgery, 222, 735-742.
- Smith, L. J., Price, D. A., & Houston, I. B. (1984). Objective structured clinical examination compared with other forms of student assessment. Archives of Disease in Childhood, 59, 1173-1176.
- Objective Structured Clinical Examination Home (OSCE Home)
http://www.oscehome.com
Copy and paste the text below:
Chan C.(2009) Assessment: Objective Structured Clinical Examination, Assessment Resources@HKU, University of Hong Kong [http://ar.talic.hku.hk]: Available: Accessed: DATE
